| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 15, Number 11, November 2024, pages 330-334
Transcatheter Closure of a Patent Foramen Ovale With a Small Adjacent Atrial Septal Defect and a Double Interatrial Septum Post Cryptogenic Stroke
Michaela Kyriakoua, d, Christos Rotosa, Thrasos Constantinidesb, Demetris Taliotisc, Christos Eftychioua
aCardiology Department, Nicosia General Hospital, Nicosia, Cyprus
bNicosia Heart Center, Nicosia, Cyprus
cUniversity Hospitals of Bristol and Weston
dCorresponding Author: Michaela Kyriakou, Cardiology Department, Nicosia General Hospital, 2029 Nicosia, Cyprus
Manuscript submitted July 16, 2024, accepted September 12, 2024, published online October 10, 2024
Short title: Transcatheter Closure of a PFO Post Stroke
doi: https://doi.org/10.14740/jmc4296
| Abstract | ▴Top |
The phenomenon of double interatrial septum (DIAS) represents a particularly rare subtype of atrial septal malformation, characterized by the presence of dual membranes separating the atria, resulting in a distinctive interatrial space. This unique anatomical structure has been linked to a paradoxical right-to-left shunt, potentially contributing to embolic ischemic strokes. Within this context, we report a rare case of a 34-year-old female who presented with a transient ischemic attack (TIA) and was diagnosed with patent foramen ovale (PFO) and a small adjacent atrial septal defect (ASD), along with the presence of a DIAS. The diagnosis was confirmed wit transoesophageal echocardiography and cardiac magnetic resonance imaging (MRI), and the condition was successfully treated with a transcatheter occluder device.
Keywords: Double interatrial septum; Patent foramen ovale; Ischemic stroke; Transcatheter occlusion; Atrial septal defect
| Introduction | ▴Top |
Double interatrial septum (DIAS) represents a rare congenital anomaly which is frequently asymptomatic, often detected incidentally during routine examination. This condition is characterized by the presence of an accessory atrial membrane running parallel to the interatrial septum, creating a distinct interatrial space. However, there are cases where it may coexist with other congenital conditions, such as patent foramen ovale (PFO) and atrial septal defect (ASD), which can predispose patients to paradoxical embolic events.
Within this framework, we present an unusual case of a 34-year-old female who presented with transient ischemic attack (TIA) of cryptogenic origin. Subsequent imaging modalities, including transesophageal echocardiography (TEE) and cardiac magnetic resonance imaging (MRI), revealed the coexistence of both DIAS and PFO, thereby elucidating the etiology of the embolic events. The patient was treated with transcatheter occlusion using an occluder device to eliminate the interatrial space and the PFO. Despite the lack of established guidelines regarding the management of this complex and rare anatomical variant, transcatheter closure should be considered when appropriate indications are present and the potential benefits outweigh the possible complications.
In this case report, we present an exceptional anatomical variant, the complexity of which poses significant challenges for clinicians in determining the optimal treatment strategy. The rarity of this condition, combined with the limited number of cases reported in the current literature, makes it difficult to establish clear management guidelines. By sharing our experience, we aim to provide new insights into the diagnosis and treatment of this rare condition.
| Case Report | ▴Top |
A 34-year-old female presented at the emergency department with acute onset left-sided numbness and weakness. She reported a similar episode 1 month prior, characterized by right-sided limb numbness, which spontaneously resolved within a few hours. The patient’s medical history included recurrent migraine episodes and three uneventful pregnancies, with no notable cardiovascular risk factors. A 12-lead electrocardiogram indicated normal sinus rhythm. As the patient’s clinical condition improved on the first day of admission, she was hospitalized in the Neurology Ward with a provisional diagnosis of a TIA. Brain MRI revealed two small embolic foci in the right frontoparietal region, suggestive of acute-subacute infarction. The patient received dual antiplatelet therapy with aspirin and clopidogrel along with atorvastatin.
Further investigations included thrombophilia screening, which was negative except for heterozygosity for MTHFR 667 C->T, and tests for antiphospholipid syndrome, which were also negative.
To explore the cryptogenic nature of the stroke, a TEE was performed to assess potential cardiac sources of emboli. The TEE revealed the presence of a mobile atrial septal aneurysm (ASA) with a 10 mm deviation from the septal midline, along with the unexpected finding of an accessory membrane, indicating the presence of two parallel structures separated by an echo-free interatrial space. These findings prompted suspicion of a DIAS, observed in the mid-esophageal short-axis view at the level of the aortic valve (Fig. 1). Additionally, color Doppler imaging demonstrated a spontaneous left-to-right shunt, suggestive of a small-sized ASD (Fig. 2), coexisting with a PFO (Fig. 3). During the Valsalva maneuver, a right-to-left shunt was observed following the injection of agitated saline contrast (Fig. 3). All pulmonary veins drained normally without any abnormal connections. Cardiac MRI confirmed the diagnosis, revealing a significant aneurysm of the septum primum (SP), accompanied by a sizable membrane (accessory atrial septum (AAS)) within the left atrium (LA) (Fig. 4a, b), further supporting the diagnosis a DIAS.
 Click for large image | Figure 1. Two-dimensional transesophageal echocardiogram (mid-esophageal short axis view at the level of AV) showing a double interatrial septum with an aneurysmal interatrial SP and an AAS with an echo-free interatrial chamber (asterisk) between them. AAS: accessory atrial septum; AV: aortic valve; LA: left atrium; RA: right atrium; SP: septum primum. |
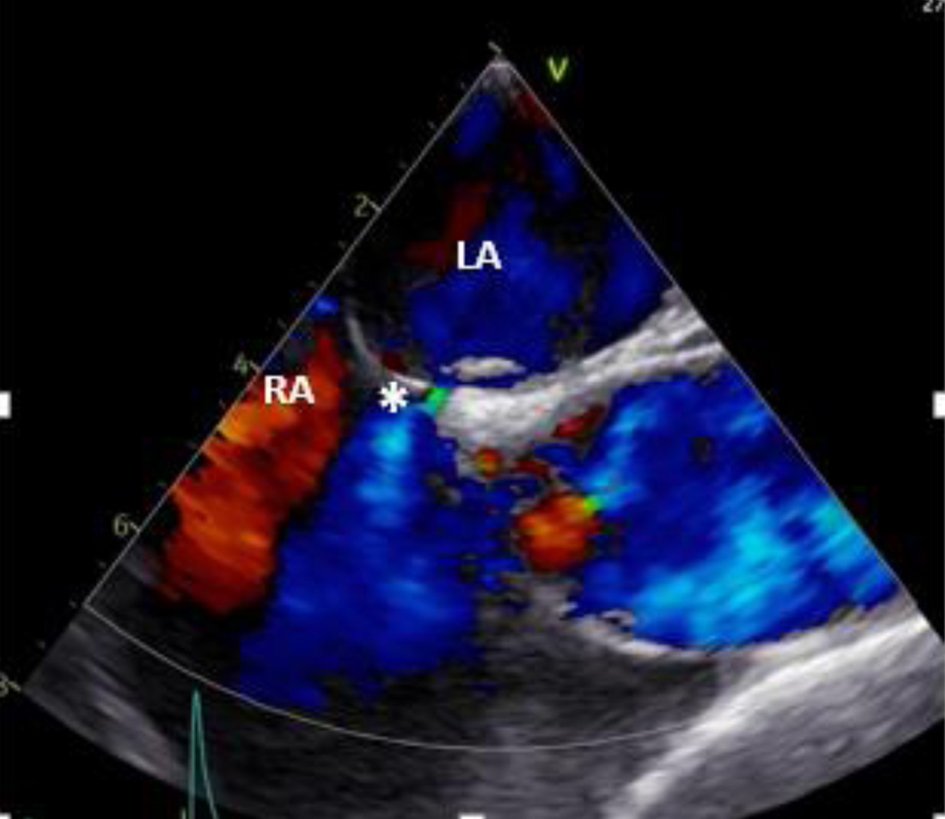 Click for large image | Figure 2. Two-dimensional transesophageal echocardiogram (mid-esophageal) in color Doppler showing flow from LA to the RA through a small-sized ASD (asterisk). ASD: atrial septa defect; LA: left atrium; RA: right atrium. |
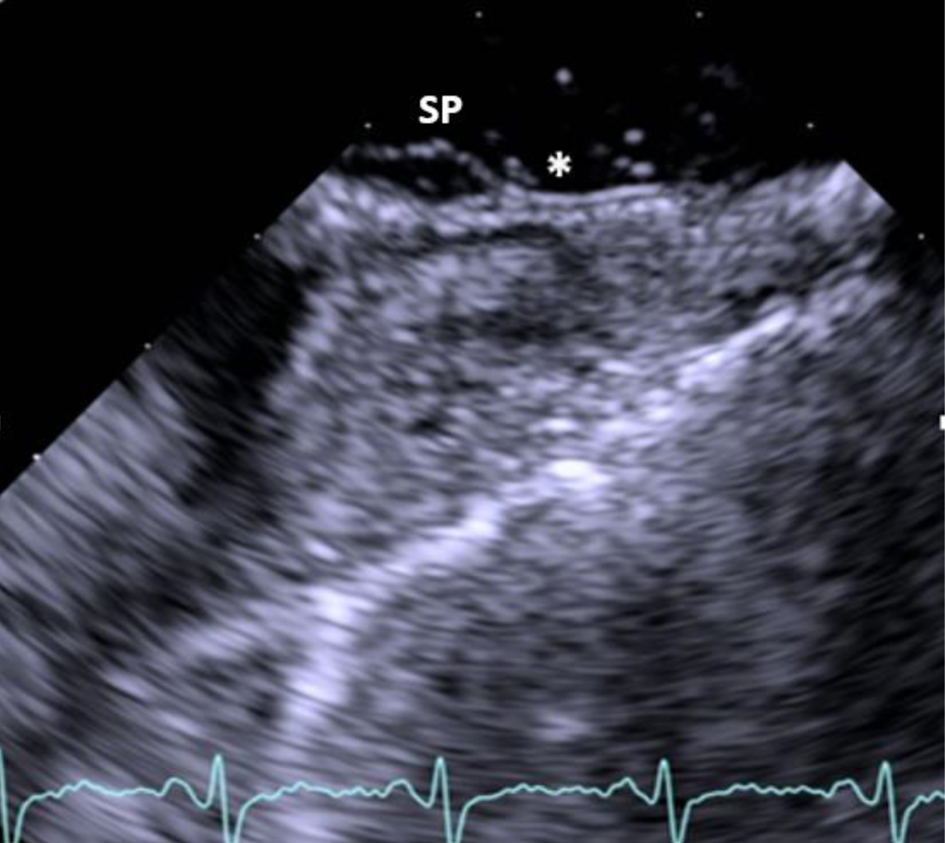 Click for large image | Figure 3. Two-dimensional transesophageal echocardiogram showing the aneurysmal SP and the presence of patent foramen ovale with right to left shunt (asterisk) after injection of agitated saline contrast during Valsalva. SP: septum primum. |
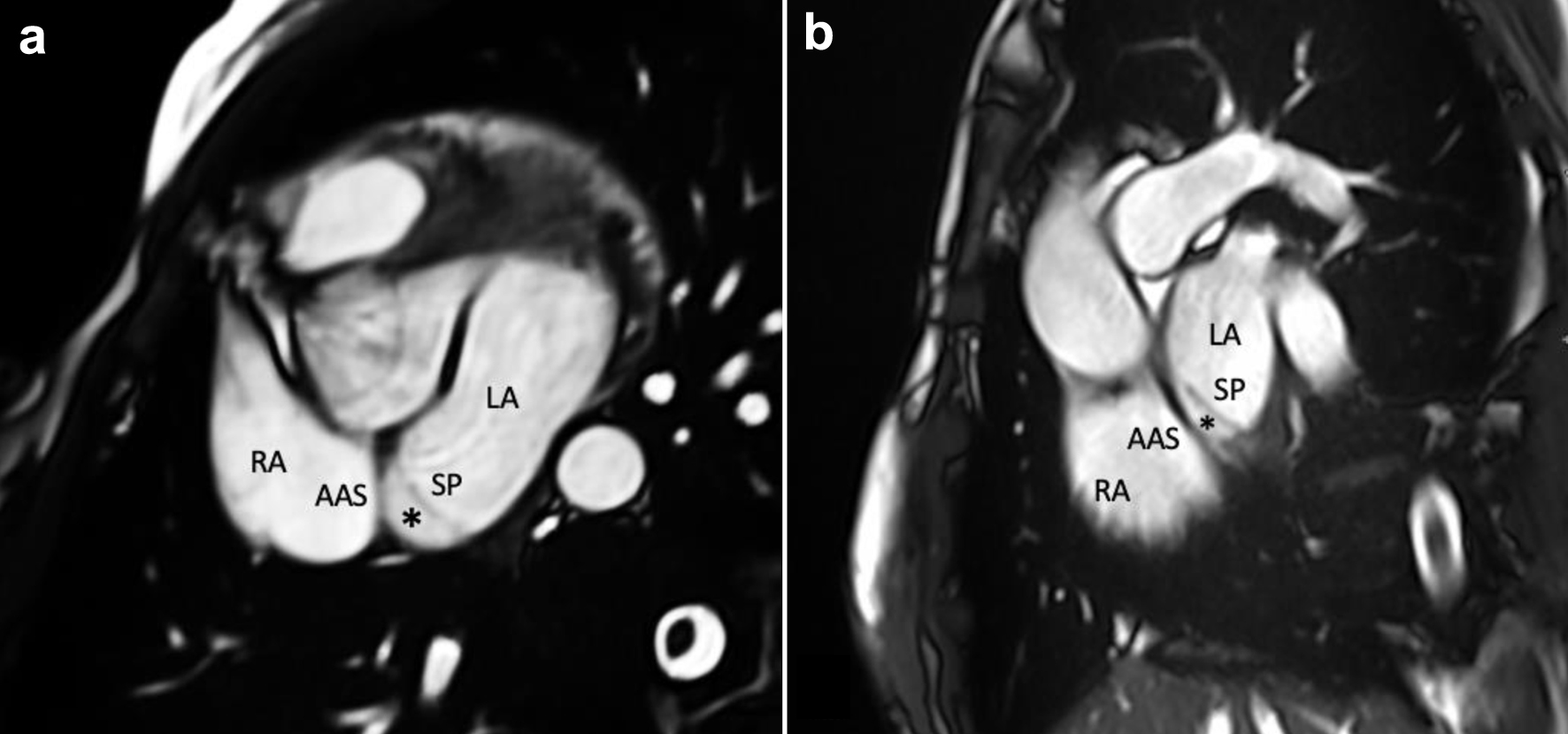 Click for large image | Figure 4. CMR imaging showing an aneurysmatic, mobile interatrial SP, an AAS and an interatrial chamber (asterisk) between them. (a) Trans-axial cine stack using bSSFP sequences. (b) Trans-axial oblique sagittal atrial cine stack using bSSFP sequences. AAS: accessory atrial septum; bSSFP: balanced steady-state free precession; CMR: cardiovascular magnetic resonance; LA: left atrium; RA: right atrium; SP: septum primum. |
The patient underwent transcatheter occlusion of the PFO/ASD, which involved the implantation of a 30 mm Occlutech Figulla Flex II PFO device (Occlutech GmbH, Jena, Germany). Initially, a 25 mm Occlutech balloon was advanced through the PFO and inflated until color Doppler confirmed cessation of flow through the PFO, as verified by periprocedural TEE. Two balloon waists were identified, with the inlet defect measuring 15 mm and the outlet defect measuring 12 mm, as observed by both fluoroscopy (Fig. 5) and TEE imaging. Subsequently, a 30 mm Occlutech Figulla Flex II PFO device was deployed with the left atrial and right atrial disks appropriately positioned on either site of the septal membranes and uncovered (Fig. 6a, b), thereby effectively bringing together the two membranes. The procedure was completed without any complications.
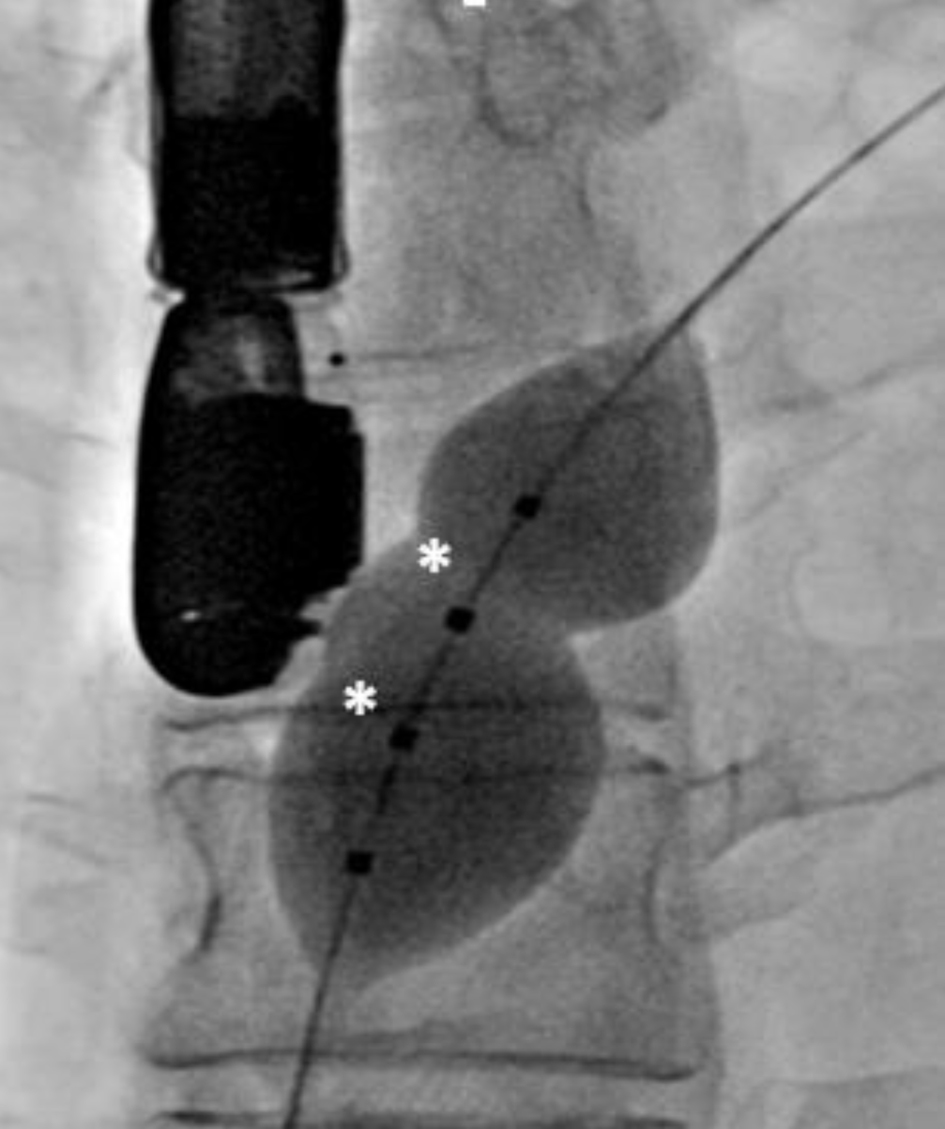 Click for large image | Figure 5. Figure 5. Fluoroscopy shows a dilated 25 mm Occlutech balloon placed through patent foramen ovale with the identification of two balloon waists (asterisks). |
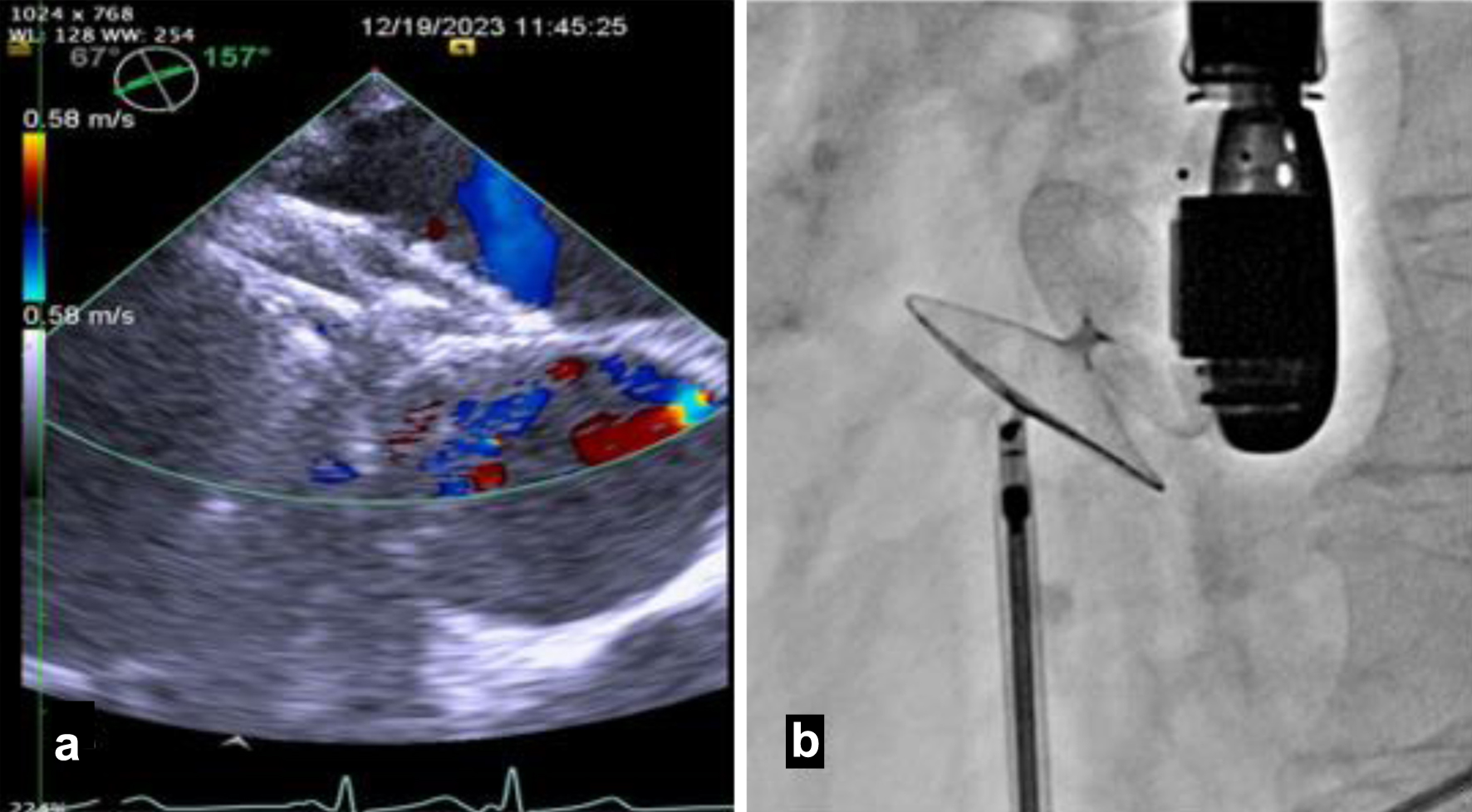 Click for large image | Figure 6. The 30 mm Occlutech Figulla Flex II PFO device was inserted, with the left atrial and right atrial disks appropriately positioned and visualized on transesophageal echocardiogram (a) and fluoroscopy (b). PFO: patent foramen ovale. |
The post-closure transthoracic echocardiogram confirmed the presence of a stable PFO closure device in place, with no evident residual shunt (Fig. 7). Upon discharge, the patient was prescribed dual antiplatelet therapy (aspirin and clopidogrel) for 3 months, followed by lifelong aspirin therapy. During subsequent follow-up evaluations at our outpatient clinic, the patient remained asymptomatic and, notably, had been migraine-free to date.
 Click for large image | Figure 7. Two-dimensional transthoracic echocardiogram (subxiphoid view) shows a well-seated patent foramen ovale closure device (red asterisk). |
| Discussion | ▴Top |
This case is novel due to the coexistence of DIAS and PFO, both of which contributed to paradoxical embolic events leading to a cryptogenic TIA. The decision to perform transcatheter closure of the interatrial space and PFO/ASD represents a rare and complex therapeutic approach, highlighting the importance of individualized treatment strategies in the absence of established guidelines for managing such rare anatomical variants.
PFO is the most prevalent congenital heart abnormality, with an incidence of 25% to 30% in the general population [1]. In contrast, DIAS is an extremely rare congenital condition characterized by a dual-layered atrial septum, resulting in the formation of a distinctive midline interatrial chamber. This chamber is usually separated from the LA by the SP and from the right atrium by an AAS [2]. The interatrial space may communicate with the LA through fenestrations such as a PFO and with the right atrium via an accessory atrial septal fenestration (ASF) [3]. The embryological development of DIAS is uncertain, but two prevailing theories explain its formation. One theory suggests it arises from incomplete perforation and resorption of the superior portion of the SP [4]. Alternatively, this condition may rarely arise from the persistent presence of the left venous valve, a remnant of the embryological sinus venosus [5].
Patients with DIAS typically remain asymptomatic and its presence is usually an incidental finding. However, they may be prone to cardioembolic events due to a large interatrial communication and a paradoxical right to left embolism. There is an additional risk of thrombosis within the accessory interatrial chamber due to blood stasis, often caused by unidirectional blood flow from high pressure chamber (LA) to the midline chamber through defects in the SP [6]. Given the rarity of cases, established guidelines for antithrombotic treatment are currently lacking. However, the prevention of thromboembolic events with oral anticoagulation over aspirin, even in the absence of atrial fibrillation, is reasonable, since the blood stasis is the primary mechanism for thrombus formation.
There is currently no standardized treatment or risk assessment protocol for the management of cardiac sources of embolism in cases of DIAS associated with stroke. However, given the concurrence with PFO/ASD, along with our patient’s recurrent ischemic events, the identification of two ischemic regions on imaging, we opted to interfere effectively through transcatheter occlusion of both DIAS and PFO. For the PFO, the current indication for the percutaneous closure entails cases with a definitive diagnosis of cryptogenic stroke, TIA or systemic embolism in individuals aged 18 and 65 years, who are presumed to have a high probability of the PFO’s contributing role [7]. In accordance with this, the primary tool utilized is the Risk of Paradoxical Embolism (RoPE) score, a predictive index that leverages easily obtainable clinical variables to assess whether a PFO is likely stroke-related or incidental in patients with cryptogenic stroke [8]. Key variables in this assessment include younger age, the absence of conventional cardiovascular risk factors, and the presence of cortical infarction on imaging [8]. In our case, the score was determined to be 9, indicating an 88% chance that stroke is due to PFO, accompanied by a 2% risk of stroke or TIA recurrence within 2 years. Among this subset of patients, percutaneous closure of PFO with implantable occluder device characterized by an “umbrella-like” double-disc design has demonstrated superior efficacy compared to medical therapy alone [9]. In our case, the coexistence of DIAS presented additional challenges for transcatheter occlusion, particularly due to the complexity of crossing the PFO and the potential persistence of an interatrial space, which could serve as a source for thrombus formation. However, we successfully crossed the accessory membrane on the first attempt using a standard guidewire, without the need for electrocautery. The DIAS was fully approximated using the Occlutech device, resulting in no residual interatrial chamber or shunt. Periprocedural imaging with TEE, in combination with fluoroscopy, was crucial for guiding the procedure, facilitating the accurate selection of an appropriately sized occlusion device, and minimizing the risk of complications [10]. In this case, the complex anatomy, including the presence of an ASD, ASA, and DIAS, necessitated the use of balloon-sizing to precisely determine the defect size and choose the most suitable occlusion device.
According to the literature, the complication rate for such procedures is approximately 7% [11], with potential complications including device embolization, atrioventricular block, cardiac perforations and erosions, atrial fibrillation, and infection [12].
Conclusion
The rare coexistence of DIAS and PFO in a symptomatic patient presenting with stroke or TIA demands careful attention, regarding the preference of transcatheter occlusion as an efficient therapeutic strategy. The diagnostic process mandates advanced imaging modalities, particularly TEE as well as cardiac MRI, to accurately identify the intricate anatomical structures involved and to guide the feasibility of percutaneous intervention. Further research and consensus guidelines are needed to optimize management and patient outcomes in this challenging clinical context.
Learning points
DIAS either alone or coexisting with a PFO, can be a rare yet significant cause of cryptogenic stroke and clinicians should be aware of this congenital abnormality. Advanced imaging modalities, including echo bubble studies, TEE and cardiac MRI, are essential tools for guiding the final diagnosis. Transcatheter occlusion constitutes a minimally invasive procedure with a low risk of complications and can be considered a therapeutic option in selected cases.
Acknowledgments
None to declare.
Financial Disclosure
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare that they have no competing interests.
Informed Consent
Written informed consent was obtained from the patient.
Author Contributions
MK, CE, and DT participated in patient care, writing of the case report, revisions, and submission process. MK, CE, and DT participated in patient care, writing of the case report and revisions. TC and CR participated in imaging. MK participated in writing of the case reports and revisions.
Data Availability
All data in our report were obtained from the patient’s hospitalization. Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
| References | ▴Top |
- Naqvi N, McCarthy KP, Ho SY. Anatomy of the atrial septum and interatrial communications. J Thorac Dis. 2018;10(Suppl 24):S2837-S2847.
doi pubmed pmc - Robaei D, Buchholz S, Feneley M. Double inter-atrial septum: a rarecause of cardioembolic stroke. Heart Lung Circ. 2013;22:315-316.
- Roberson DA, Javois AJ, Cui W, Madronero LF, Cuneo BF, Muangmingsuk S. Double atrial septum with persistent interatrial space: echocardiographic features of a rare atrial septal malformation. J Am Soc Echocardiogr. 2006;19(9):1175-1181.
doi pubmed - Javois AJ, Roberson DA. Unusual atrial septal anatomy resulting in an interatrial chamber: the true triatrial heart? Pediatr Cardiol. 2007;28(3):224-228.
doi pubmed - Van Praagh R, Corsini I. Cor triatriatum: pathologic anatomy and a consideration of morphogenesis based on 13 postmortem cases and a study of normal development of the pulmonary vein and atrial septum in 83 human embryos. Am Heart J. 1969;78(3):379-405.
doi pubmed - Molisana M, Cicchitti V, Bagicalupi E, Ianni U, Procopio A, Toro A, Parato V, et al. C44 atrial septal abnormalities: a case of double interatrial septum. European Heart Journal Supplements. 2023;25(Supplement):D19.
doi - Pristipino C, Sievert H, D'Ascenzo F, Louis Mas J, Meier B, Scacciatella P, Hildick-Smith D, et al. European position paper on the management of patients with patent foramen ovale. General approach and left circulation thromboembolism. Eur Heart J. 2019;40(38):3182-3195.
doi pubmed - Kent DM, Ruthazer R, Weimar C, Mas JL, Serena J, Homma S, Di Angelantonio E, et al. An index to identify stroke-related vs incidental patent foramen ovale in cryptogenic stroke. Neurology. 2013;81(7):619-625.
doi pubmed pmc - Sperlongano S, Giordano M, Ciccarelli G, Bassi G, Malvezzi Caracciolo D'Aquino M, Del Giudice C, Gaio G, et al. Advances in percutaneous patent foramen ovale closure: from the procedure to the echocardiographic guidance. J Clin Med. 2022;11(14):4001.
doi pubmed pmc - Fraisse A, Latchman M, Sharma SR, Bayburt S, Amedro P, di Salvo G, Baruteau AE. Atrial septal defect closure: indications and contra-indications. J Thorac Dis. 2018;10(Suppl 24):S2874-S2881.
doi pubmed pmc - Brown KN, ElBebawy B, Shah AH, Kanmanthareddy A. Catheter management of patent foramen ovale. In: StatPearls. Treasure Island (FL). 2024.
pubmed - Yang MC, Wu JR. Recent review of transcatheter closure of atrial septal defect. Kaohsiung J Med Sci. 2018;34(7):363-369.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


