| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 3, Number 3, June 2012, pages 161-163
Skeletal Langerhans Cell Histiocytosis Presenting After Periodontal Disease and Diabetes Insipidus: A Case Report
John D Smitha, Daniel E Portera, James S Huntleyb, c
aNew Royal Infirmary of Edinburgh, Little France, Old Dalkeith Road, Edinburgh EH16 4SU, UK
bRoyal Hospital for Sick Children, Dalnair Street, Yorkhill, Glasgow G3 8SJ, UK
cCorresponding author: James S Huntley
Manuscript accepted for publication December 14, 2011
Short title: Atypical Presentation of Langerhans Cell Histiocytosis
doi: https://doi.org/10.4021/jmc476w
| Abstract | ▴Top |
Langerhans Cell Histiocytosis (LCH) is a rare condition with extreme clinical variability in terms of presentation, progression and outcomes. A case is described in which Diabetes Insipidus (DI) and periodontal disease preceded the development of a lesion of the temporal bone. Central DI in the child or young adult should prompt an extracranial survey for possible LCH. Periodontal disease has a marked association with LCH, so when DI and periodontal disease co-exist, the index of suspicion for LCH should be raised.
Keywords: Langerhans cell histiocytosis; Diabetes insipidus; Periodontal disease
| Introduction | ▴Top |
Langerhans Cell Histiocytosis (LCH) is a rare condition with extreme variability in presentation, progression and outcomes. It is characterised by the proliferation of dendritic cells (Langerhans Cells) normally concerned with antigen presentation [1, 2]. LCH has an estimated incidence of 2 to 5 cases per million per year [2], recently given as 4.1 cases per million per year for children in the United Kingdom aged 0 - 14 years [3]. First described by Alfred Hand in 1893 [4, 5], LCH has been loosely and incompletely categorised into several eponymous and non-eponymous conditions [6]: (1) eosinophilic granuloma of bone; (2) Hand-Schüller-Christian Disease (triad of exophthalmos, skull defects and diabetes insipidus (DI)) and (3) Letterer-Siwe Disease (acute, progressive multisystem infiltration in the very young, < 3 years of age).
The presenting features are variable in both adult and paediatric groups [7] but isolated bone lesions are a common mode of presentation in both age groups, and have excellent prospects of disease free survival after treatment [7, 8]. Multi-system variants have variable clinical findings - including dyspnoea, diabetes insipidus, hepatosplenomegaly, hypothyroidism, mucous membrane (especially oral) lesions and skin rashes [9]. LCH in adults (in contrast to the condition in children) tends to be a multisystem disease, but the highest mortality is seen in those with isolated pulmonary involvement [7].
DI is a rare presenting feature in solitary system disease but more common in multisystem disease - in the recent UK case series of 94 patients aged 0 - 14 years, 69 (73%) had single system disease, of whom only 2 had pituitary involvement; conversely of the 25 multisystem cases, 5 had DI [3]. Overall, 17-25% of children with LCH develop DI (10 - and references therein). In the situation of a child/young adult carrying a diagnosis of central DI, LCH was found in 12 out of 79 patients (15%) [11]. Therefore, though rare, central diabetes insipidus should raise the possibility of an underlying diagnosis of LCH [11], and an extracranial survey (with a view to identifying other sites of LCH which may be more amenable to biopsy) has been advocated [12].
Several authors have focussed on periodontal and gingival disease in LCH [13-17] because the incidence of oral lesions is high - 77% has been quoted [17], though Annibali et al (2009) described a series of 31 LCH patients of whom 12 (namely 39%) developed oral lesions [16]. When oral lesions and DI co-exist in the same patient, there should be a strong index of suspicion for LCH.
| Case Report | ▴Top |
A 27 year old female salesperson was referred with a three week history of severe pain - including night pain - and tenderness in the region of her right temple in December 2000. There was no history of trauma. Her past medical history included extremely poor dentition since childhood and Diabetes Insipidus (DI), diagnosed in 1993, for which she took daily intranasal desmopressin acetate. Blood tests, including erythrocyte sedimentation rate, full blood count, urea and electrolytes, and liver function tests, were within reference ranges.
Skull X-rays showed a well demarcated lucent area of approximately 2 cm diameter in the right temporal bone and evidence of periodontal disease (Fig. 1). Temporal excision biopsy was performed, with histology showing Langerhans Cell Histiocytosis (LCH).
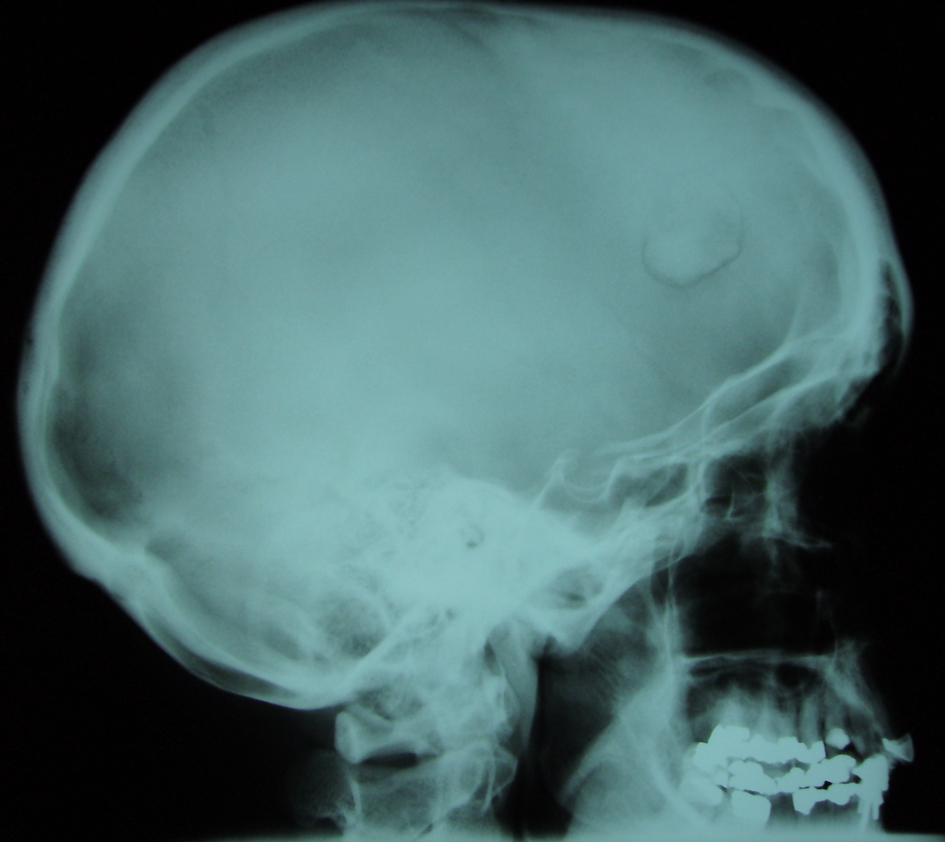 Click for large image | Figure 1. Lateral skull radiograph. There is a temporal bone lesion with a curved well-demarcated lucency. There has been a large amount of dentistry indicative of oral/periodontal disease. |
In April 2003, the patient developed severe atraumatic pain in her right groin, which was worse on walking and also at night. Examination demonstrated a tender focal area overlying the greater trochanter. Blood tests were again unremarkable. Radiographs showed a lucent area in the greater trochanter. Curettage of the lesion allowed histological confirmation of LCH recurrence at this site.
Due to long-term dentition problems, a phased dental clearance was initiated in February 2004, leading to a significant improvement in the patient’s quality of life. No granulomas were demonstrated in tissue cleared - however it is considered likely that LCH was implicated at this site also. Similarly, later curettage of a possible right iliac crest lesion (2005) was not confirmed as LCH on histology. She remains free of further LCH recurrence (2010) and continues to take desmopressin for her DI.
| Discussion | ▴Top |
Our patient had an uncommon presentation of a rare condition - central diabetes insipidus (DI) associated with extremely poor dentition/gingival disease. Until the emergence of more typical localised bone pain in her skull and orthopaedic referral, the possibility of LCH had not been considered.
In conclusion, LCH is a rare and enigmatic condition [18], which infrequently presents as central DI. Clinicians encountering a combination of DI and gingival disease should consider the possibility of LCH, and investigate further.
Consent
Written informed consent was obtained from the patient for publication of this case report and the accompanying image. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Grant Funding
None.
Conflict of Interest
The authors declare that they have no competing interests.
Abbreviations
LCH: Langerhans cell histiocytosis; DI: diabetes insipidus
| References | ▴Top |
- Garg S, Mehta S, Dormans JP. Langerhans cell histiocytosis of the spine in children. Long-term follow-up. J Bone Joint Surg Am. 2004;86-A(8):1740-1750.
pubmed - Leonidas JC, Guelfguat M, Valderrama E. Langerhans' cell histiocytosis. Lancet. 2003;361(9365):1293-1295.
pubmed doi - Salotti JA, Nanduri V, Pearce MS, Parker L, Lynn R, Windebank KP. Incidence and clinical features of Langerhans cell histiocytosis in the UK and Ireland. Arch Dis Child. 2009;94(5):376-380.
pubmed doi - Hand A. Polyuria and tuberculosis. Arch Pediatr. 1893;10:673-675.
- Hand A. Defects of membranous bones, exophthalmos and polyuria in childhood; is it dyspituitarism? Am J Med Sci. 1921;162:509-515.
- Lichtenstein L. Histiocytosis X; integration of eosinophilic granuloma of bone, Letterer-Siwe disease, and Schuller-Christian disease as related manifestations of a single nosologic entity. AMA Arch Pathol. 1953;56(1):84-102.
pubmed - Howarth DM, Gilchrist GS, Mullan BP, Wiseman GA, Edmonson JH, Schomberg PJ. Langerhans cell histiocytosis: diagnosis, natural history, management, and outcome. Cancer. 1999;85(10):2278-2290.
pubmed doi - Islinger RB, Kuklo TR, Owens BD, Horan PJ, Choma TJ, Murphey MD, Temple HT. Langerhans' cell histiocytosis in patients older than 21 years. Clin Orthop Rel Res. 2000;379:231-235.
- Arico M, Girschikofsky M, Genereau T, Klersy C, McClain K, Grois N, Emile JF, et al. Langerhans cell histiocytosis in adults. Report from the International Registry of the Histiocyte Society. Eur J Cancer. 2003;39(16):2341-2348.
pubmed doi - Carpinteri R, Patelli I, Casanueva FF, Giustina A. Pituitary tumours: inflammatory and granulomatous expansive lesions of the pituitary. Best Pract Res Clin Endocrinol Metab. 2009;23(5):639-650.
pubmed doi - Maghnie M, Cosi G, Genovese E, Manca-Bitti ML, Cohen A, Zecca S, Tinelli C, et al. Central diabetes insipidus in children and young adults. N Engl J Med. 2000;343(14):998-1007.
pubmed doi - Prosch H, Grois N, Prayer D, Waldhauser F, Steiner M, Minkov M, Gadner H. Central diabetes insipidus as presenting symptom of Langerhans cell histiocytosis. Pediatr Blood Cancer. 2004;43(5):594-599.
pubmed doi - Artzi Z, Grosky M, Raviv M. Periodontal manifestations of adult onset of histiocytosis X. J Periodontol. 1989;60(1):57-66.
pubmed doi - Muzzi L, Pini Prato GP, Ficarrat G. Langerhans' cell histiocytosis diagnosed through periodontal lesions: a case report. J Periodontol. 2002;73(12):1528-1533.
pubmed doi - Mortellaro C, Pucci A, Palmeri A, Lucchina AG, Berta M, Celeste A, Costantino S, et al. Oral manifestations of langerhans cell histiocytosis in a pediatric population: a clinical and histological study of 8 patients. J Craniofac Surg. 2006;17(3):552-556.
pubmed doi - Annibali S, Cristalli MP, Solidani M, Ciavarella D, La Monaca G, Suriano MM, Lo Muzio L, et al. Langerhans cell histiocytosis: oral/periodontal involvement in adult patients. Oral Dis. 2009;15(8):596-601.
pubmed doi - Madrigal-Martinez-Pereda C, Guerrero-Rodriguez V, Guisado-Moya B, Meniz-Garcia C. Langerhans cell histiocytosis: literature review and descriptive analysis of oral manifestations. Med Oral Patol Oral Cir Bucal. 2009;14(5):E222-228.
pubmed - Iupati D, Chander S. A case report of langerhans histiocytosis presenting sequentially over a 21-year period with Letterer-Siwe disease, hand-Schuller-Christian disease and eosinophillic granuloma of bone. J Pediatr Hematol Oncol. 2006;28(11):746-749.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


