| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 3, March 2013, pages 146-148
Proptosis, Diplopia, and an Ocular Bruit in a Patient With Ehlers-Danlos Syndrome
Donald P Mebusta, b, Jordan A Zeiglera
aKaiser Permanente San Diego Medical Center, USA
bCorresponding author: Donald P Mebust, Kaiser Permanente San Diego Medical Center, USA
Manuscript accepted for publication October 25, 2012
Short title: Ehlers-Danlos Syndrome
doi: https://doi.org/10.4021/jmc915w
| Abstract | ▴Top |
We describe a case of a 30-year-old female with a history of the Vascular form of Ehlers-Danlos Syndrome who presented to a community Emergency Department with complaints of eye pain, blurred vision, and diplopia. On examination, she was noted to have proptosis, scleral injection and an ocular bruit. Imaging studies demonstrated dissection of the carotid artery and a carotid cavernous sinus fistula. Patient underwent endovascular coil embolization of the lesion with resolution of symptoms.
Keywords: Ehlers-Danlos; Carotid cavernous sinus fistula; Proptosis
| Introduction | ▴Top |
Ehlers-Danlos Syndrome (EDS) is a rare hereditable group of connective tissue disorders with an estimated prevalence of one in every 10,000 to 25,000 births [1]. It is characterized by genetic mutations and subsequent deficits in collagen synthesis. The latest classification describes 6 major types, which are based on clinical and genetic presentations [2]. While all 6 types may have some degree of bleeding diathesis, Type IV, now referred to as the Vascular form, is well known for its catastrophic, vascular complications. This rare and lethal form of EDS is associated with ruptured blood vessels, aneurysms, dissections, fistulas and spontaneous ruptures of the uterus and gastrointestinal structures.
We present a case of a direct spontaneous carotid cavernous sinus fistulas (CCF) in patient with the Vascular form of EDS. This neurovascular complication results from rupture of a weakened carotid artery into the cavernous sinus. Increased pressure inside the cavernous sinus produces headaches, cranial nerve palsies, visual disturbance, tinnitus, proptosis and venous hypertension in ocular and cerebral vessels. Untreated, it can lead to permanent vision loss and devastating intracranial hemorrhage.
| Case Report | ▴Top |
A 30-year-old female with history of Vascular type of Ehlers-Danlos syndrome presented to a community Emergency Department with 2 months of pulsatile tinnitus in the right ear and temporal region and right sided ocular discomfort. Four weeks prior to presentation, she was seen by her primary care physician with these progressing complaints. She was diagnosed with Eustachian tube dysfunction and was treated with nasal steroids. Her symptoms continued, and one week prior to admission to the Emergency Department, she developed progressive periorbital discomfort, scleral injection and blurred vision. She was seen again in primary care and received a diagnosis of conjunctivitis. On the day of presentation to the Emergency Department, she developed diplopia and proptosis.
On presentation, she was in moderate distress complaining of a severe headache and eye pain. She described a “swishing sound” in her head. Her blood pressure was 130/80 in the right upper extremity and 138/85 in the left upper extremity. Her heart rate was 100 beats per minute and respiratory rate was 18 with an oxygen saturation of 98% on room air. Her visual acuity was 20/40 in the left eye and 20/80 in the right eye. She had proptosis of the right eye with scleral injection. Auscultation over the right eye revealed an ocular bruit. On fundoscopic exam, the patient had prominent retinal veins but no hemorrhages. Examination of left eye was unremarkable. Her cardiac exam demonstrated normal heart sounds without any murmurs. Her abdomen was soft without palpable masses. Cranial nerve exam showed a right CNVI palsy and ocular pain with eye movement. Neurological exam was otherwise unremarkable.
The patient was sent for an emergent unenhanced, CT scan of the brain and orbits, which revealed dilatation of the ophthalmic vein and exophthalmos. The patient was then taken emergently for an MRI/MRA/MRV of the brain and neck, which revealed a dilated ophthalmic vein, spontaneous dissection of the internal carotid artery at the level of the petrous portion of the temporal bone, a direct carotid cavernous fistula, and engorged cerebral veins (Fig. 1).
 Click for large image | Figure 1. MRI/MRA/MRV of the brain revealed a dilated ophthalmic vein (long arrow), engorged cerebral veins (short arrows), spontaneous dissection of the internal carotid artery at the level of the petrous portion of the temporal bone (short arrow) and a direct carotid cavernous fistula (long arrow). |
Our patient was taken to the angiography suite for emergent, endovascular treatment. The fistula was successfully embolized with transvenous, intracavernous platinum coils placed via the ipsilateral inferior petrosal venous sinus (Fig. 2).
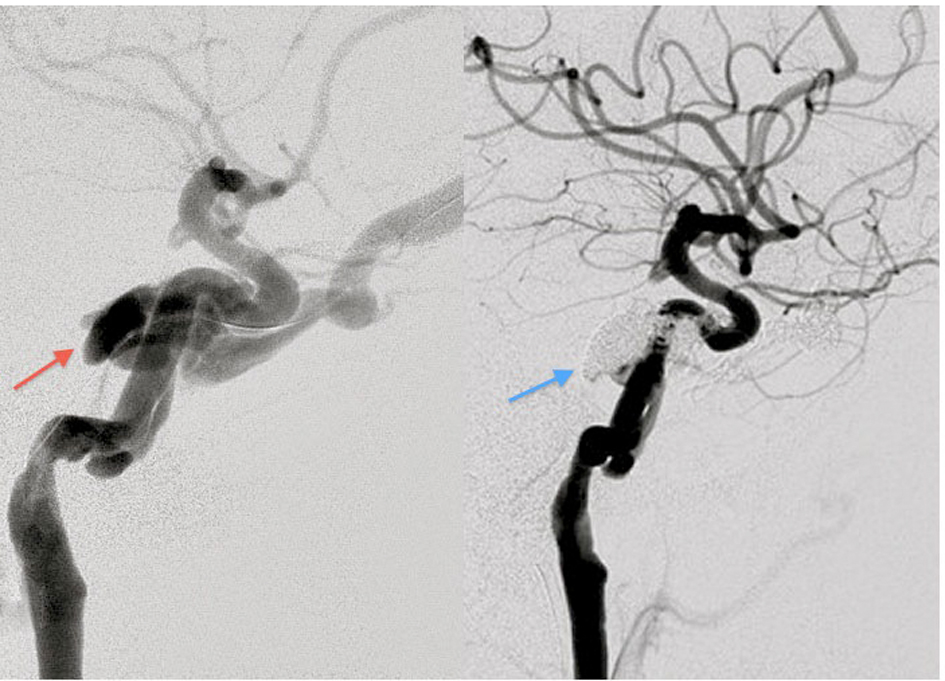 Click for large image | Figure 2. The fistula prior to embolization (red arrow). Fistula status post coil embolization (blue arrow). |
She had immediate resolution of the pulsatile tinnitus and rapid resolution of her ocular symptoms. At one month follow up, the she continued to have mild diplopia with lateral gaze, but was otherwise symptom free.
| Discussion | ▴Top |
Ehlers-Danlos Syndrome (EDS) is a group of inherited connective tissue disorders with 6 subtypes. Estimated prevalence is between 1/10,000 and 1/25,000. The Vascular type of EDS (also known as Type lV) represents 4% of cases. It results from the mutation in the COL3A1 gene. This defect leads to reduced collagen lll, which is a major constituent of vessel walls as well as the uterus and gastrointestinal structures. Complications of Vascular EDS include vascular ruptures, dissections, and aneurysms of medium and large caliber vessels. Nonvascular complications include uterine rupture and spontaneous rupture of hollow and solid viscera. While rare in childhood, these complications affect 25% of the patients before the age of 20 and 80% by the age of 40. Arterial ruptures result in the majority of deaths with a median death at age 50 [1].
Our patient suffered from the vascular complication known as spontaneous carotid cavernous sinus fistula (CCF). Although posttraumatic CCF is well documented in the literature, spontaneous CCF associated with EDS is far more rare. In 2004, Mitsuhashi et al reported only 33 previously documented cases worldwide [3].
CCF results from an abnormal connection between the internal or external carotid artery and the venous system of the cavernous sinus. Abnormal collagen deposition in the arterial media of the carotid artery leads to aneurysmal formation, and eventual rupture into the cavernous sinus. Increased pressure in the cavernous sinus leads to compression of cavernous contents and congestion of the ophthalmic venous system. This leads to the symptoms of tinnitus, ocular pain, chemosis, opthalmoplegia, diplopia and proptosis. In addition, reflux of arterialized blood into cerebral cortical veins can lead to rupture and CNS hemorrhage [4].
Diagnosis of CCF requires a high clinical suspicion in patients presenting with these symptoms. A personal or family history of Ehlers-Danlos Syndrome should heighten this concern. Emergency Department work-up should include an emergent CT of the brain and orbits and emergent Neurointerventional Surgery consultation. An MR brain and orbits with MR angiogram and MR venogram provide superior sensitivity and direct visualization of the fistula. Findings include dilated ophthalmic veins, proptosis, retrobulbar fat stranding, cavernous sinus dilatation, and the presence of a fistula.
Historically, palliative ligation of the carotid artery was the therapy of choice. Transarterial balloon embolization was then introduced in the 1980’s affording closure of the fistula with preservation of a patent carotid artery. Unfortunately, complication rates remained high. Secondary to the thin, fragile nature of the arterial walls, these patients suffered dissections and ruptures at the site of repair and along the entire course of the catheterized artery. Schievink et al reported a 35% morbidity rate and a 12% mortality rate with diagnostic angiography alone. Intervention carried an additional 17% mortality [5]. Halbach et al reported similar poor outcomes with a 50% morbidity rate and a 25% mortality rate [6].
The high risk of therapy had led many to question the benefits of intervention. Some have even recommended conservative management of CCF, which can be complicated by potential blindness and fatal intracranial bleeding. Fortunately, advancements in endovascular surgery have shown promising results. Transvenous coil embolization has replaced intraarterial balloon embolization. This allows the use of smaller catheters with softer tips and avoidance of arterial manipulation and trauma. Recent case reports have demonstrated improved outcomes [7-11].
Despite operative risks, the decision was made to treat our patient with transvenous embolization. CCF rarely resolves spontaneously in patients with Vascular form of EDS. Untreated, it would have lead to permanent vision loss. In addition, the arterialized cerebral veins placed her at eminent risk of intracranial hemorrhage. Our patient was treated with 19 transvenous platinum coils. She did remarkably well with no vascular injury, and had immediate improvement in her symptoms. At one month follow up she demonstrated mild cranial nerve Vl nerve palsy but was otherwise asymptomatic. She will be managed on an aspirin a day for treatment of her non-flow limiting internal carotid dissection, and a beta blocker which is believed to offer a 3 fold reduction in further vascular complications [12]. Follow up MRI brain and neck will be performed at 6 month intervals.
| References | ▴Top |
- Germain DP. Ehlers-Danlos syndrome type IV. Orphanet J Rare Dis. 2007;2:32.
doi pubmed - Beighton P, De Paepe A, Steinmann B, Tsipouras P, Wenstrup RJ. Ehlers-Danlos syndromes: revised nosology, Villefranche, 1997. Ehlers-Danlos National Foundation (USA) and Ehlers-Danlos Support Group (UK). Am J Med Genet. 1998;77(1):31-37.
doi - Mitsuhashi T, Miyajima M, Saitoh R, Nakao Y, Hishii M, Arai H. Spontaneous carotid-cavernous fistula in a patient with Ehlers-Danlos syndrome type IV—case report. Neurol Med Chir (Tokyo). 2004;44(10):548-553.
doi - Hollands JK, Santarius T, Kirkpatrick PJ, Higgins JN. Treatment of a direct carotid-cavernous fistula in a patient with type IV Ehlers-Danlos syndrome: a novel approach. Neuroradiology. 2006;48(7):491-494.
doi pubmed - Schievink WI, Piepgras DG, Earnest Ft, Gordon H. Spontaneous carotid-cavernous fistulae in Ehlers-Danlos syndrome Type IV. Case report. J Neurosurg. 1991;74(6):991-998.
doi pubmed - Halbach VV, Higashida RT, Dowd CF, Barnwell SL, Hieshima GB. Treatment of carotid-cavernous fistulas associated with Ehlers-Danlos syndrome. Neurosurgery. 1990;26(6):1021-1027.
doi pubmed - Kanner AA, Maimon S, Rappaport ZH. Treatment of spontaneous carotid-cavernous fistula in Ehlers-Danlos syndrome by transvenous occlusion with Guglielmi detachable coils. Case report and review of the literature. J Neurosurg. 2000;93(4):689-692.
doi pubmed - Lach B, Nair SG, Russell NA, Benoit BG. Spontaneous carotid-cavernous fistula and multiple arterial dissections in type IV Ehlers-Danlos syndrome. Case report. J Neurosurg. 1987;66(3):462-467.
doi pubmed - Chuman H, Trobe JD, Petty EM, Schwarze U, Pepin M, Byers PH, Deveikis JP. Spontaneous direct carotid-cavernous fistula in Ehlers-Danlos syndrome type IV: two case reports and a review of the literature. J Neuroophthalmol. 2002;22(2):75-81.
doi pubmed - Van Overmeire O, De Keukeleire K, Van Langenhove P, Defreyne L. Carotid-cavernous fistula in ehlers-danlos syndrome by pure transvenous approach. Interv Neuroradiol. 2006;12(1):45-51.
pubmed - Lum YW, Brooke BS, Black JH, 3rd. Contemporary management of vascular Ehlers-Danlos syndrome. Curr Opin Cardiol. 2011;26(6):494-501.
doi pubmed - Ong KT, Perdu J, De Backer J, Bozec E, Collignon P, Emmerich J, Fauret AL, et al. Effect of celiprolol on prevention of cardiovascular events in vascular Ehlers-Danlos syndrome: a prospective randomised, open, blinded-endpoints trial. Lancet. 2010;376(9751):1476-1484.
doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


