| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 12, Number 7, July 2021, pages 280-283
Primary Osteosarcoma of the Urinary Bladder Metastatic to Lung
Amira Elwya, b, Amr Solimana, Mohamed Mahera, Yasmin Abdelhakama, Ali Saada, Mohamed Ahmed Abdul Latif Elsayedc, Mohamed El-Kaffasd, Noha Rashadd, e, Nesreen Magdya, f, g
aPathology Department, Shefaa Al-Orman Oncology Hospital, Luxor, Egypt
bPathology Department, South Egypt Cancer Institute, Assiut University, Egypt
cRadiology Department, Shefaa Al-Orman Oncology Hospital, Luxor, Egypt
dMedical Oncology Department, Shefaa Al-Orman Oncology Hospital, Luxor, Egypt
eResearch Department, Armed Forces College of Medicine, Egypt
fPathology Department, National Cancer Institute, Cairo University, Egypt
gCorresponding Author: Nesreen Magdy, Histopathology Department, Shefaa Al-Orman Oncology Hospital, New City of Tiba, Downtown District, Luxor, Egypt
Manuscript submitted October 31, 2020, accepted April 13, 2021, published online May 13, 2021
Short title: Primary Urinary Bladder Osteosarcoma
doi: https://doi.org/10.14740/jmc3613
| Abstract | ▴Top |
Extra-skeletal osteosarcoma (ESOS) is a rare neoplasm that represents less than 2% of all soft tissue sarcomas. Common reported sites of involvement include limbs, retroperitoneum, chest wall and buttocks. ESOS arising primarily in parenchymatous organs are extremely uncommon, with the involvement of the urinary bladder is even rarer. We herein report a case of primary ESOS of the urinary bladder in a 48 year-old male patient.
Keywords: Urinary bladder; Osteosarcoma; Bone forming tumors; Lung metastases; SATB2
| Introduction | ▴Top |
Extra-skeletal osteosarcoma (ESOS) is a rare neoplasm that represents less than 2% of all soft tissue sarcomas [1]. Common reported sites of involvement include limbs, retroperitoneum, chest wall and buttocks [2]. ESOS arising in parenchymatous organs is extremely uncommon [3], with the primary involvement of the urinary bladder even rarer [4]. We herein report a case of primary ESOS of the urinary bladder in a 48-year-old male patient.
| Case Report | ▴Top |
A 48-year-old male patient presented to our hospital with history of hematuria for 3 days. An abdominal ultrasound was performed and revealed a urinary bladder right anterolateral polypoid soft tissue endo-luminal fungating mass 5 × 6 cm, with central echogenic part and peripheral rod like macro-calcifications. Contrast-enhanced computed tomography (CT) scan showed a right anterolateral mural-based fungating mass lesion, measuring 60× 55 × 60 mm with extra-vesical extension and smudging of the peri-vesical fat planes. The mass spared both vesico-ureteric junctions, both semino-vesical junctions and the prostate. Small peri-vesical prominent enhancing lymph nodes were noted (Fig. 1).
 Click for large image | Figure 1. Computed tomography findings of the urinary bladder mass lesion (arrow denotes the tumor). |
A trans-uretheral biopsy was performed, and fragments weighing 2.42 g from the mass with a separate biopsy from the deep muscle weighing 1.13 g were received to the pathology laboratory. Histological examination of both biopsies (Fig. 2) revealed focally ulcerated urothelium with underlying tumor formed of sheets of non-cohesive large malignant epithelioid cells showing marked pleomorphism, hyperchromatic nuclei with bizarre and multinucleated forms. Mitotic activity was marked. Tumor cells were seen embedded in an eosinophilic osteoid matrix with focal calcification. Immunohistochemical study revealed diffuse positive reaction of the tumor cells for vimentin and SATB-2 but negative for cytokeratin (only stained the residual intact urothelium). The lack of urothelial carcinoma or carcinosarcoma components in our case has qualified the diagnosis of primary osteosarcoma.
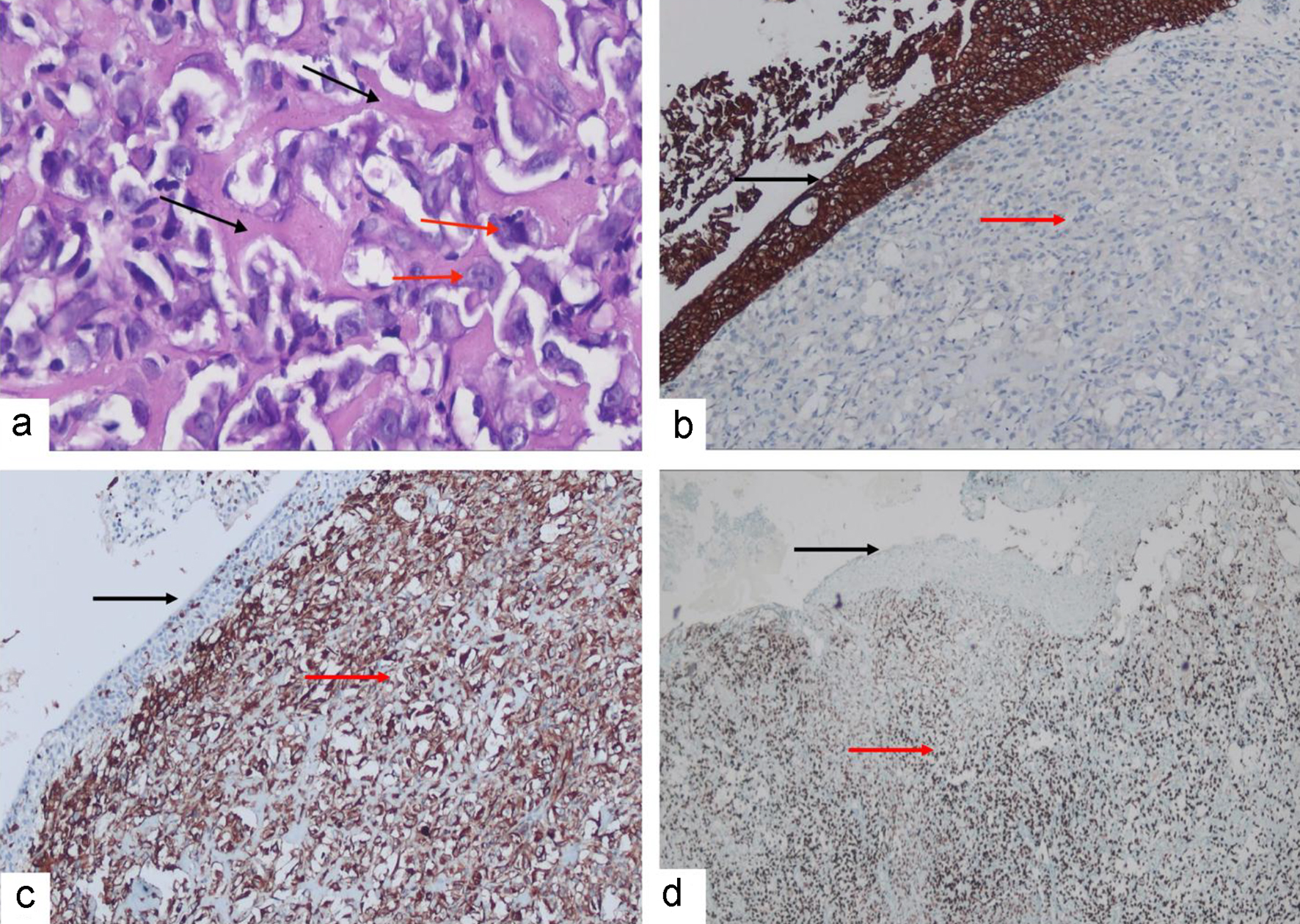 Click for large image | Figure 2. (a) Hematoxylin and eosin-stained sections reveal malignant bone forming neoplasm formed of highly anaplastic cells (red arrows) admixed with abundant lace-like malignant osteoid (black arrows). Immunostained sections reveal that tumor cells are negative for CK (red arrow) which stains the lining urothelium (black arrow) (b). Tumor cells are positive membranous and cytoplasmic immunoreactivity for vimentin (red arrow) which is negative in the surface urothelium (black arrow) (c). Tumor cells (red arrows) show nuclear positivity for SATB-2 (red arrow) which is negative in the surface urothelium (black arrow) (d). |
The patient received one cycle of cisplatin 60 mg/m2 and adriamycin 60 mg/m2, and then was admitted to the intensive care unit (ICU) with electrolytes disturbance.
Follow-up chest CT after 1 month revealed multiple bilateral scattered pulmonary nodules, some of which were calcified with the largest noted at the anterior segment of the right upper lobe of lung measuring about 2.5 cm, likely metastatic. The patient lost to follow-up 2 months after diagnosis.
| Discussion | ▴Top |
ESOS is a rare mesenchymal neoplasm, first described in 1941. It represents 1-2% of all soft tissue sarcomas [1] and 2-5% of all osteosarcomas [3]. Unlike conventional osteosarcoma, ESOS is more frequent among elders [5]. Histologically, ESOS is classified into the same subtypes of the skeletal osteosarcoma [6].
Reported sites involved by ESOS include limbs, retroperitoneum, chest wall and breast. In the latter, ESOS is distinguished from matrix-producing carcinomas by the lack of any epithelial component [2]. Primary urinary bladder sarcomas are uncommon and comprise < 1% of all urinary bladder malignancies [7], and osteosarcomas in particular are exceedingly rare [8]. It is more common in males than in females with a male to female ratio of 4:1, and usually presents with hematuria [4, 8].
The main differential diagnosis of urinary bladder ESOS is sarcomatoid carcinoma and urothelial carcinomas with osseous metaplasia [9]. In our case, the histology was identical to conventional bone osteosarcoma with the characteristic lace-like osteoid, calcification and osteoid-related osteoblastic cells of marked pleomorphism. The sections were totally lacking any evidence of an epithelial component. Additionally, the tumor cells were diffusely positive for SATB-2 and vimentin, but negative for CK. However, the distinction from carcinosarcoma does not have major therapeutic implications, as both tumors require aggressive therapy, yet the distinction from low-grade urothelial carcinoma with osseous metaplasia is important [8].
Surgery is the standard of care for management of localized ESOS. The role of systemic chemotherapy remains controversial with no comparative studies conducted due to rarity of disease. The currently available evidence comes from retrospective cohorts with small size.
A case series published in 2005 suggested improved outcome of ESOS patients receiving multi-agent chemotherapy protocols of conventional osteosarcoma for localized disease [10]. Another study suggested superiority of osteosarcoma-type chemotherapy (methotrexate, cisplatin, doxorubicin and ifosfamide) compared to soft tissue sarcoma-type chemotherapy (anthracycline-based +/- ifosfamide chemotherapy) in the perioperative setting [2]. Data on metastatic disease remain very limited.
A trend towards improvement of progression-free survival/overall survival (PFS/OS) was reported in patients receiving platinum-based chemotherapeutic regimens [11]. However, these findings were recently challenged by results of large studies [5, 12].
A retrospective SEER database analysis recently reported including 310 patients presented between 1975 and 2016, making it the largest series up till now [5], showed no specific effect for chemotherapy on prognosis. However, this study included only 51 cases with visceral ESOS. Old age, visceral primary site, no surgical resection and distant metastases were poor prognostic factors [5]. Data on targeted therapy for ESOS are very limited.
Based on the previous data, and due to controversial findings and absence of high-grade evidence, systemic chemotherapy is usually adapted with either a platinum-based combination or osteosarcoma-type chemotherapy [10].
ESOS is a high-grade sarcoma with poor prognosis. In relatively large cohort studies of patients with ESOS, the 5-year OS is less than 50% for localized tumors and less than 30% for metastatic patients [2]. ESOS has a high recurrence rate after resection that reported to be as high as 50% [1, 3]. There are several reported poor prognostic factors that include patient age > 40 years, relatively large tumor size > 5 cm, retroperitoneal and intra-abdominal tumors, positive margins, regional lymph node involvement and distant metastasis [2, 3]. The most common cause of death is distant metastasis, with the lung being the most common site [7].
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
Research concept and design: NM. Collection and/or assembly of data: NM, MS, MEK, ASo, MM, YA, ASa. Data analysis and interpretation: NM, MEK. Writing the article: NM, AE, MEK. Preparations of figures and figure legends: AE, MS, ASo, MM, YA, ASa. Critical revision of the article: NM, AE, MS, NR, MEK, ASo, MM, YA, ASa. Final approval of article: NM, AE, MS, NR, MEK, ASo, MM, YA, ASa.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Klein MJ, Siegal GP. Osteosarcoma: anatomic and histologic variants. Am J Clin Pathol. 2006;125(4):555-581.
doi - Longhi A, Bielack SS, Grimer R, Whelan J, Windhager R, Leithner A, Gronchi A, et al. Extraskeletal osteosarcoma: A European Musculoskeletal Oncology Society study on 266 patients. Eur J Cancer. 2017;74:9-16.
doi pubmed - Saadaat R, Abdul-Ghafar J, Ud Din N, Haidary AM. Anal extraskeletal osteosarcoma in a man: a case report and review of the literature. J Med Case Rep. 2020;14(1):51.
doi pubmed - Degirmencioglu S, Sen Turk N, Herek D, Tuncay L. Case report synchronous osteosarcoma of the bladder and adenocarcinoma of the colon: a case report. Int J Clin Exp Med. 2018;11(9):10092-10095.
- Qi L, Wan L, Ren X, Zhang W, Tu C, Li Z. The role of chemotherapy in extraskeletal osteosarcoma: a propensity score analysis of the surveillance epidemiology and end results (SEER) database. Med Sci Monit. 2020;26:e925107.
doi - Fletcher C, Bridge J, Hogendoorn P, Mertens F, eds. Extraskeletal osteosarcoma. In: WHO classification of tumours of soft tissue and bone 4th ed. Lyon: IARC Press; 2013:161-162.
- Almadani N, Alsaad KO, Al-Matrafi H, Al Hadab A, Abdullah N, AlKushi A. Urinary bladder radiotherapy-related chondroblastic osteosarcoma: Rare case report and review of literature. Urol Ann. 2014;6(3):247-250.
doi pubmed - Ghalayini IF, Bani-Hani IH, Almasri NM. Osteosarcoma of the urinary bladder occurring simultaneously with prostate and bowel carcinomas: report of a case and review of the literature. Arch Pathol Lab Med. 2001;125(6):793-795.
doi pubmed - S G, NF D, MA A, JT MR, Thornhill J. Primary osteosarcoma of the urinary bladder. Open J Clin Med Case Reports. 2016;2(8):1106.
- Goldstein-Jackson SY, Gosheger G, Delling G, Berdel WE, Exner GU, Jundt G, Machatschek JN, et al. Extraskeletal osteosarcoma has a favourable prognosis when treated like conventional osteosarcoma. J Cancer Res Clin Oncol. 2005;131(8):520-526.
doi pubmed - Paludo J, Fritchie K, Haddox CL, Rose PS, Arndt CAS, Marks RS, Galanis E, et al. Extraskeletal osteosarcoma: outcomes and the role of chemotherapy. Am J Clin Oncol. 2019;41(9):832-837.
doi pubmed - Liao Z, Qiu M, Yang J, et al. Outcomes of surgery and/or combination chemotherapy for extraskeletal osteosarcoma: a single-center retrospective study from China. Sci Rep. 2019;9(1):1-8.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


