| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 4, April 2023, pages 124-129
Rapidly-Progressing Pyomyositis After Chest Contusion in a Patient With Well-Controlled Diabetes Mellitus
Kazuya Uraa, c, Misato Motoyab, Hidehiro Ishiib
aDepartment of General Internal Medicine, Saiseikai Futsukaichi Hospital, Fukuoka, Japan
bDepartment of Diabetology, Saiseikai Futsukaichi Hospital, Fukuoka, Japan
cCorresponding Author: Kazuya Ura, Department of General Internal Medicine, Saiseikai Futsukaichi Hospital, Chikushino-City, Fukuoka-Prefecture 818-8516, Japan
Manuscript submitted April 11, 2023, accepted April 26, 2023, published online April 30, 2023
Short title: Rapidly-Progressing Pyomyositis
doi: https://doi.org/10.14740/jmc4099
| Abstract | ▴Top |
Pyomyositis is an uncommon acute bacterial infection of the skeletal muscle. It is sometimes referred to as “tropical pyomyositis” because it has been primarily reported as an endemic disease in tropical regions. In temperate climates, it is mainly diagnosed in immunocompromised persons, such as those with human immunodeficiency virus infection, malignancy, diabetes, and various other medical conditions. Early diagnosis and appropriate antimicrobial therapy for pyomyositis are important, however, it is often missed in its early stage. Herein, we report the case of a patient with obesity and well-controlled diabetes in whom rapid onset pyomyositis developed in only 2 days after chest contusion and induced bacteremia in its early stage. He was successfully treated by antimicrobials without any drainage or surgical intervention. Even in patients with well-controlled diabetes or in healthy persons, pyomyositis should be considered for patients who present with fever and muscle swelling and pain, especially when they have obesity and a history of blunt trauma. It should also be noted that pyomyositis, mimicking muscle contusion or hematoma can appear very early after blunt muscle trauma. Prompt diagnosis and antimicrobial treatment for pyomyositis can lead to a favorable outcome, without surgical drainage.
Keywords: Pyomyositis; Diabetes; Obesity; Muscle trauma; Methicillin-sensitive Staphylococcus aureus
| Introduction | ▴Top |
Pyomyositis is a rare, acute bacterial infection of the skeletal muscle [1, 2] that is referred to as “tropical pyomyositis” because it has been primarily reported as an endemic disease in tropical regions. Most cases of tropical pyomyositis tend to occur in otherwise healthy persons, and the majority of cases in temperate regions are immunocompromised persons or those who have serious comorbidities, such as human immunodeficiency virus infection, malignancy, immunosuppressive therapy, organ transplantation, liver cirrhosis, diabetes mellitus (DM), renal insufficiency, or intravenous drug abuse [1-3]. Local muscle trauma and strenuous exercise are predisposing factors for pyomyositis, which are seen in 25-50% of patients [1]. Staphylococcus aureus (S. aureus) is the most common etiologic pathogen of pyomyositis, reported in 90% of tropical cases and up to 75% of temperate cases [1]. It is often missed in its early stage, and the delay of diagnosis and appropriate treatment results in increased morbidity and mortality [4]. Recently, pyomyositis has been reported to have increased in temperate climates because of the rising number of immunocompromised persons [2]. Here we describe a rare case of pyomyositis of the pectoralis major that occurred very early after chest contusion in a patient with obesity and well-controlled DM.
| Case Report | ▴Top |
Investigations
A 49-year-old Japanese man visited our hospital complaining of 2 days of fever and left precordial chest pain. He had stumbled 5 days prior to admission, bruising his left front chest when he fell to the ground. His body temperature 2 days later was over 40.0 °C, and the severity of the left anterior chest pain increased. He presented to the emergency department of our hospital 4 days after the fall. His anterior left chest was edematous and tender, and his blood examination revealed a C-reactive protein level of 22.12 mg/dL. He was admitted to our hospital the next day, and ampicillin-sulbactam (ABPC/SBT) was given intravenously because of a suspected infection.
The patient had a medical history of DM, which had been diagnosed approximately 5 years earlier. His DM had been recently treated with metformin, vildagliptin, and dapagliflozin, and his recent hemoglobin A1c (HbA1c) level was continuously below 7.0%. Additional medical history included hypertension and dyslipidemia. He reported that he occasionally drank alcohol and did not smoke.
Physical examination revealed an erythematous, tender, and swollen left anterior chest. His blood pressure was 107/66 mm Hg, heart rate 95 beats per minute, axillary temperature 37.5 °C, and oxygen saturation (SpO2) 95% while breathing ambient air. The body mass index (weight in kilograms divided by height in meters squared) was 38.0 kg/m2. Auscultation of the chest revealed no murmur. The skin examination revealed erythema, swelling, and tenderness over his left anterior chest.
The patient’s white blood cell count was 10,300/µL, with 85% neutrophils. A liver function test revealed aspartate aminotransferase (AST) 136 U/L, alanine aminotransferase (ALT) 138 U/L, and total bilirubin (T-Bil) 2.0 mg/dL. Blood urea nitrogen (BUN) was 15.7 mg/dL and creatinine 0.93 mg/dL. The serum CRP level was 22.12 mg/dL. The creatinine kinase level was normal (Table 1).
 Click to view | Table 1. Laboratory Data on Admission |
Computed tomography (CT) of the chest without contrast material showed swelling of the left major pectoralis muscle and its surrounding subcutaneous fat (Fig. 1a).
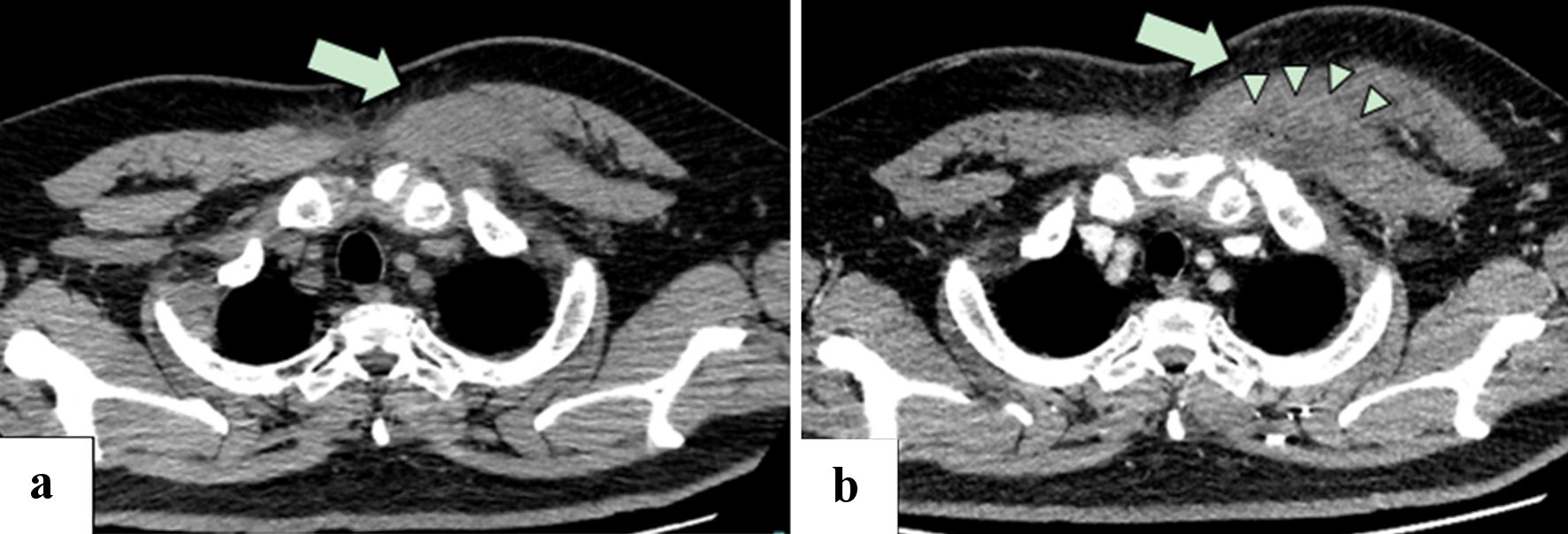 Click for large image | Figure 1. (a) Plain CT of the chest 1 day before admission showed swelling of the left major pectoralis muscle, with subcutaneous fat stranding (arrow). (b) Contrast-enhanced CT of the chest on day 3 of hospitalization showed a poor contrast enhancement area in the swelling of the major pectoralis muscle with ring-enhancement (arrow) and minute gas production (arrow heads), suggesting abscess formation. Left pleural effusion was revealed. CT: computed tomography. |
Diagnosis
On day 3 of admission, the fever and continuous chest pain persisted, and CT of the chest was performed after the administration of intravenous contrast material, which revealed a poor contrast enhancement area in the swollen pectoralis major muscle with ring-enhancement and minute gas production, suggesting abscess formation (Fig. 1b). There was no evidence of liquified abscess or distant metastatic disease, thus, no surgical drainage or debridement was done.
Treatment
The same day, Gram-positive cocci was grown from the blood culture, and vancomycin was added to ABPC/SBT. Based on this, he was diagnosed with pyomyositis of the left pectoralis major muscle.
On day 4 of admission, bacteria from blood culture were identified as methicillin-sensitive S. aureus (MSSA), so the antimicrobial was changed to cefazolin. Repeated blood cultures were negative, and a transthoracic echocardiogram was normal. Magnetic resonance imaging (MRI) performed on day 10 of hospitalization showed a low-signal intensity area in T1-weighted imaging and a high-signal intensity area in T2-weighted images, short tau inversion recovery (STIR) images, and diffusion-weighted imaging (DWI) in the left pectoralis major muscle (Fig. 2a, c), suggesting inflammation and abscess formation.
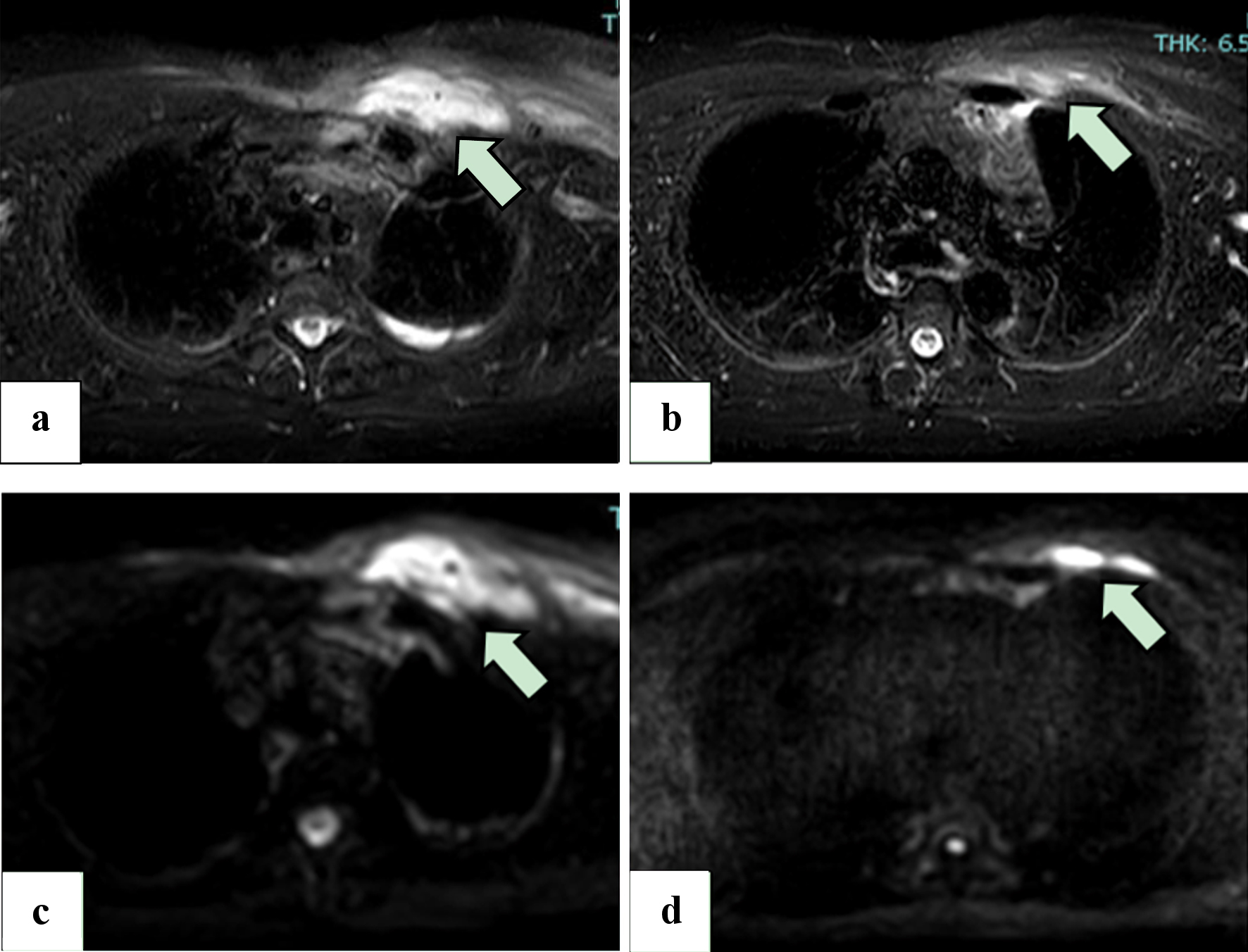 Click for large image | Figure 2. (a, b) STIR images from the MRI scan on day 10 of hospitalization (a) and 11 days after hospital discharge (b), without intravenous administration of gadolinium. Areas of high signal (arrow) reduction indicate that the swelling of the left pectoralis major has improved. (c, d) DWI MRI scans of the chest on day 10 of hospitalization (c) and 11 days after hospital discharge (d), without intravenous administration of gadolinium. The volume of the abscesses in the pectoralis major muscle (arrow) has been reduced. MRI: magnetic resonance imaging; STIR: short tau inversion recovery; DWI: diffusion-weighted imaging. |
Sliding scale insulin therapy was initiated for the treatment of DM, which was then switched to oral agents (vildagliptin 100 mg/day, metformin hydrochloride 1,000 mg/day, and dapagliflozin 5 mg/day). During admission, his blood glucose level showed good control (fasting blood glucose of 108 - 150 mg/dL). A total of 14 days of intravenous antimicrobial therapy was given, followed by oral cefalexin 500 mg orally three times a day. His symptoms gradually improved, and he was discharged 15 days after being admitted.
Follow-up and outcomes
At outpatient follow-ups, repeated MRI of the chest showed decreased area of inflammation and reductions in size of the abscess (Fig. 2b, d), and he completed a total of 6 weeks of antimicrobial therapy. He showed full recovery with no recurrence after cessation of antimicrobial therapy.
| Discussion | ▴Top |
We presented a case of rapidly-progressing pyomyositis of the pectoralis major muscle after chest contusion in a patient with obesity and well-controlled DM. The present case has several important features, well-controlled DM, rapid disease progression after blunt muscle trauma, and a favorable outcome without surgical drainage. The successful cure of this patient was due to prompt diagnosis and treatment.
Pyomyositis is an uncommon disease in temperate regions, where it has been recognized as a disease in immunocompromised persons [1-3]; however, it is sometimes seen in patients with well-controlled DM and even in healthy persons, especially in patients with obesity or blunt muscle trauma. As in the present case, pyomyositis can present a rapidly-progressing clinical course and can be difficult to distinguish from simple traumatic changes.
The present case had DM, a risk factor for pyomyositis. His DM was well-controlled, which suggested he was not severely immunocompromised. About one-third of patients with pyomyositis had DM in various reports [3, 5, 6]; however, the association between the severity of DM and the risk of pyomyositis is poorly documented. While muscle trauma probably contributed to the development of the pyomyositis of the present patient, it alone was not considered to be sufficient to explain the disease. The HbA1c level was 6.7% and he did not have other comorbidities that would predispose him to infection, which suggests that even patients with well-controlled DM might be at risk of pyomyositis. DM might be a predisposing factor for pyomyositis, though it may not be due to hyperglycemia-related impairment of the immune response but also to the colonization of S. aureus, which is associated with transient bacteremia, or to vascular insufficiency due to macro- and microangiopathy. Furthermore, the duration of time a patient has DM may be important, because long-term DM causes microangiopathy, which leads to muscle ischemia and infarction that renders muscles susceptible to bacterial infection. Recently, obesity has been reported to be a risk factor for pyomyositis, independently from DM [2]. Although the DM of this patient was well-controlled, a combination of DM, obesity, and blunt muscle trauma might have induced his pyomyositis. The rapid onset seen in the present case suggests that transient S. aureus bacteremia occurred almost simultaneously with the muscle trauma.
It is difficult to make a correct diagnosis of pyomyositis in its early stage. A mean delay of 10 days from the onset of the symptom to a correct diagnosis of pyomyositis [7] and that pyomyositis is often missed at early stage [3] have been reported. Clinical presentations in early stage pyomyositis, such as skin erythema, swelling, and tenderness, make it difficult to distinguish pyomyositis from cellulitis or necrotizing fasciitis. Furthermore, it is especially difficult for patients with blunt muscle trauma to distinguish pyomyositis from a traumatic change such as a muscle contusion or hematoma, as in the present case. Even CT or MRI is not definitive because early stage pyomyositis often shows only inflammatory changes, not abscesses. Laboratory findings are nonspecific, and creatine kinase levels are typically normal. In the present case, pyomyositis developed in only 2 days after the chest contusion. Furthermore, he developed bacteremia only 5 days after the chest contusion. The disease progression of this patient was more rapid than the course seen in a previous report [8]. It is important to diagnose this disease in its earliest stages because a delay of treatment can induce bacteremia and infectious endocarditis, which can result in sepsis, a need for amputation or surgical drainage, or even in death. Early diagnosis and appropriate antimicrobial therapy can prevent complications and reduce the need for surgical drainage, as in the present case.
A representative study [8] reported that pyomyositis can be divided into three stages, with the first stage typically subacute (Table 2) [8-10]. Although the current situation is different from that of 1970s from Nigeria, that report presents the natural course of pyomyositis and has been referred to by many other reports about pyomyositis [1, 3, 4, 9-13]. The present case was diagnosed during stage 1, then rapidly progressed to stages 2 - 3 (Table 2) [8-10]. Although aspiration of pus or surgical drainage is generally needed in stage 2 to 3 pyomyositis, the present case fully recovered by antimicrobial agents alone. Indeed, previous studies with many cases have reported that more than half of patients with pyomyositis needed surgical intervention [3-6, 11]. Contrast-enhanced CT at day3 showed abscess formation but no liquid pus that could be punctured and drained, thus pus aspiration or surgical drainage was not performed. The present case shows that prompt diagnosis and antimicrobial treatment can make it possible to manage pyomyositis by antimicrobial therapy alone, without surgical drainage.
 Click to view | Table 2. Clinical Stages of Pyomyositis [8-10] and the Clinical Course of the Present Case |
Because of its rarity, clinical evidence for pyomyositis is derived from several case series. In these reports, the epidemiology of the etiologic pathogens is reported to be quite different between countries. For example, S. aureus has been reported to be the most common etiologic pathogen of pyomyositis in 90% of tropical cases and up to 75% of temperate cases [1]. However, patients with underlying medical conditions tend to have pyomyositis by Gram-negative bacteria [2, 4, 11], and initially these patients tended to receive inappropriate antimicrobial therapy [4].
Antimicrobial therapy should be based on epidemiological data and the patients’ underlying medical illnesses. Especially important is whether or not an anti-methicillin-resistant S. aureus (MRSA) drug should be contained in the initial empiric therapy. The guidelines of the Infectious Diseases Society of America recommend anti-MRSA empiric therapy for skin and soft tissue infections [14]. However, the proportion of MRSA as the causative organism of pyomyositis was quite different among studies; 2.9% in Korea [6], 10% [3] to 20% [2] in the USA, and 12.9% [4] to 75% in India [15]. Furthermore, studies of pyomyositis that include a large number of cases are lacking in Japan, thus the distribution of causative pathogens and the proportions of underlying medical conditions are unclear. To further appropriate initial treatment, future epidemiological studies are needed in Japan and other countries where the data of pyomyositis are scarce.
In conclusion, we have presented a case of pyomyositis of the pectoralis major muscle that progressed rapidly after chest contusion in a patient with obesity and well-controlled DM. Even in such patients, concurrent muscle trauma and transient S. aureus bacteremia can induce rapidly-progressing pyomyositis. A prompt diagnosis and antimicrobial treatment are crucial, however, pyomyositis is often missed during its early stage (stage 1). A high index of suspicion is necessary for the prompt diagnosis of pyomyositis for patients with rapidly-progressing muscle swelling and inflammatory changes, especially when they have blunt muscle trauma and obesity.
Learning points
Pyomyositis can appear very early after muscle blunt trauma even in patients without obvious immunodeficiency. DM, even if it is well-controlled, may predispose patients to pyomyositis. Early diagnosis and appropriate antimicrobial treatment for pyomyositis can lead to a favorable outcome, without surgical drainage.
Acknowledgments
None to declare.
Financial Disclosure
Authors received no specific funding.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Informed Consent
Written informed consent was obtained from the patient prior to writing this report.
Author Contributions
KU, MM, and HI participated in the patient’s treatment. KU wrote the paper. MM and HI assisted in revising the manuscript. All authors read and approved the final manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
DM: diabetes mellitus; S. aureus: Staphylococcus aureus; CRP: C-reactive protein; ABPC/SBT: ampicillin-sulbactam; HbA1c: hemoglobin A1c; AST: aspartate aminotransferase; ALT: alanine aminotransferase; T-Bil: total bilirubin; BUN: blood urea nitrogen; CT: computed tomography; MSSA: methicillin-sensitive S. aureus; MRI: magnetic resonance imaging; STIR: short tau inversion recovery; MRSA: methicillin-resistant S. aureus
| References | ▴Top |
- Chauhan S, Jain S, Varma S, Chauhan SS. Tropical pyomyositis (myositis tropicans): current perspective. Postgrad Med J. 2004;80(943):267-270.
doi pubmed pmc - Maravelas R, Melgar TA, Vos D, Lima N, Sadarangani S. Pyomyositis in the United States 2002-2014. J Infect. 2020;80(5):497-503.
doi pubmed - Burdette SD, Watkins RR, Wong KK, Mathew SD, Martin DJ, Markert RJ. Staphylococcus aureus pyomyositis compared with non-Staphylococcus aureus pyomyositis. J Infect. 2012;64(5):507-512.
doi pubmed - Kumar S, Bhalla A, Singh R, Sharma N, Sharma A, Gautam V, Singh S, et al. Primary pyomyositis in North India: a clinical, microbiological, and outcome study. Korean J Intern Med. 2018;33(2):417-431.
doi pubmed pmc - Radcliffe C, Gisriel S, Niu YS, Peaper D, Delgado S, Grant M. Pyomyositis and infectious myositis: a comprehensive, single-center retrospective study. Open Forum Infect Dis. 2021;8(4):ofab098.
doi pubmed pmc - Kim T, Park SY, Kwak YG, Jung J, Kim MC, Choi SH, Yu SN, et al. Etiology, characteristics, and outcomes of community-onset pyomyositis in Korea: a multicenter study. Infect Chemother. 2021;53(1):46-52.
doi pubmed pmc - Bickels J, Ben-Sira L, Kessler A, Wientroub S. Primary pyomyositis. J Bone Joint Surg Am. 2002;84(12):2277-2286.
doi pubmed - Chiedozi LC. Pyomyositis. Review of 205 cases in 112 patients. Am J Surg. 1979;137(2):255-259.
doi pubmed - Habeych ME, Trinh T, Crum-Cianflone NF. Purulent infectious myositis (formerly tropical pyomyositis). J Neurol Sci. 2020;413:116767.
doi pubmed - Narayanappa G, Nandeesh BN. Infective myositis. Brain Pathol. 2021;31(3):e12950.
doi pubmed pmc - Crum NF. Bacterial pyomyositis in the United States. Am J Med. 2004;117(6):420-428.
doi pubmed - Crum-Cianflone NF. Bacterial, fungal, parasitic, and viral myositis. Clin Microbiol Rev. 2008;21(3):473-494.
doi pubmed pmc - Shittu A, Deinhardt-Emmer S, Vas Nunes J, Niemann S, Grobusch MP, Schaumburg F. Tropical pyomyositis: an update. Trop Med Int Health. 2020;25(6):660-665.
doi pubmed - Stevens DL, Bisno AL, Chambers HF, Dellinger EP, Goldstein EJ, Gorbach SL, Hirschmann JV, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the infectious diseases society of America. Clin Infect Dis. 2014;59(2):147-159.
doi pubmed - Chattopadhyay B, Mukhopadhyay M, Chatterjee A, Biswas PK, Chatterjee N, Debnath NB. Tropical pyomyositis. N Am J Med Sci. 2013;5(10):600-603.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


